
Manual flipping of breast implants addresses unintended rotation or shifting, often resolved through gentle manipulation. It’s a common post-surgical issue, with smooth implants showing higher flip rates than textured ones.
1.1 Definition and Overview
Manually flipping breast implants refers to the non-surgical correction of implant malposition, where the implant rotates or shifts within the breast pocket. This phenomenon, often termed “pancake flipping,” occurs when the implant’s front side faces backward, altering its intended position. Manual correction involves external manipulation to realign the implant. Studies show smooth round implants are more prone to flipping than textured anatomical ones. This issue can lead to visible deformities or discomfort, necessitating prompt intervention to restore both aesthetics and patient comfort. Understanding this process is crucial for addressing post-surgical complications effectively.
1.2 Importance of Understanding the Issue
Understanding manual breast implant flipping is crucial for addressing post-surgical complications. Implant malposition, such as flipping or rotation, can lead to aesthetic issues, discomfort, and patient dissatisfaction. Early detection and correction are vital to prevent further complications like capsular contracture or seroma. Patients with smooth round implants are at higher risk, with a flip rate of 5.9% compared to 1.4% for textured anatomical implants. Recognizing the signs, such as unexpected shape changes or discomfort, enables timely intervention. Education and awareness for both patients and surgeons are key to improving outcomes and minimizing the need for revision surgeries;
Causes of Breast Implant Flipping
Breast implant flipping is often caused by implant design, surgical technique, and pocket size. Smooth implants are more prone to flipping than textured ones, with a higher flip rate.
2.1 Implant Type and Design
The type and design of breast implants significantly influence the likelihood of flipping. Smooth round implants are more prone to flipping due to their slippery surface, with a flip rate of 5.9% compared to 1.4% for textured anatomical implants. The structural design, including the presence of a single or double lumen, also plays a role. Textured implants tend to adhere better to surrounding tissue, reducing movement. Conversely, smooth implants can shift more easily within the breast pocket, leading to malposition. Understanding implant design helps in assessing susceptibility to flipping and guides preventive measures.
2.2 Surgical Technique and Pocket Size
The surgical technique and pocket size play a critical role in breast implant flipping. A larger pocket can allow excessive movement, increasing the risk of malposition. Proper pocket creation is essential to prevent shifting. Surgeons must ensure precise dissection and placement to maintain implant stability. Improper muscle coverage or inadequate tissue support can also contribute to flipping. Studies show that patients with larger pockets or suboptimal placement are more likely to experience implant malposition. Addressing these factors during surgery can significantly reduce the likelihood of post-operative complications, emphasizing the importance of surgical precision and tailored techniques for each patient.

Types of Breast Implant Malposition
Breast implant malposition occurs when implants shift from their intended position. Common types include flipping (pancake flipping) and rotation (door or wheel rotation), with smooth implants showing higher flip rates.
3.1 Flipping (Pancake Flipping)
Flipping, or “pancake flipping,” occurs when a breast implant rotates so the back side faces forward, altering its position and shape. This is more common in smooth implants due to their design, which allows easier movement within the breast pocket. Flipping can result from factors like improper pocket size, weak tissue support, or muscle contractions. It may cause visible deformities or discomfort, often requiring manual correction or surgical intervention. Early detection is crucial to prevent complications, with clinical examination and imaging techniques aiding diagnosis. Addressing flipping promptly ensures optimal aesthetic and functional outcomes for patients.
3.2 Rotation (Door or Wheel Rotation)
Rotation, referred to as “door” or “wheel” rotation, involves the implant turning within the breast pocket, where one side shifts upward or outward. This type of malposition is less common than flipping but can still cause noticeable asymmetry or shape changes. Smooth implants are more prone to rotation due to their design, which allows greater mobility. Factors like muscle contractions, implant placement, and pocket size contribute to this issue. While some rotations may self-correct, persistent cases often require manual adjustment or surgical intervention to restore proper alignment and aesthetic appearance. Early detection is key to preventing complications.
Clinical Characteristics and Risk Factors
Clinical characteristics include implant type, with smooth implants showing higher flip rates. Patient-related factors like muscle dynamics and device-related issues, such as pocket size, influence malposition risks.
4.1 Patient-Related Factors
Patient-related factors significantly influence breast implant flipping. Body type, muscle tone, and activity levels play a role. Patients with weaker chest muscles or larger implants are more prone to malposition. Additionally, post-surgical activities, such as heavy lifting or intense exercise, can displace implants. Genetic factors, like connective tissue strength, also contribute. Proper patient selection and lifestyle considerations are crucial to minimize risks. Understanding these factors helps in tailoring surgical approaches and post-operative care to individual needs, reducing the likelihood of implant flipping and ensuring optimal outcomes.
4.2 Device-Related Factors
Device-related factors, such as implant type and design, significantly impact flipping risks. Smooth round implants are more prone to flipping compared to textured anatomical ones, as shown in studies. The design of the implant influences its stability within the breast pocket. Larger implants or those with less cohesive gel may shift more easily. Additionally, the implant’s surface texture plays a role, with textured implants adhering better to surrounding tissue, reducing malposition. Understanding these device-specific characteristics is crucial for minimizing flipping risks and ensuring proper implant placement and stability.
Diagnosis of Breast Implant Flipping
Diagnosis involves clinical examination and imaging techniques like ultrasound or MRI to assess malposition and confirm the need for correction.
5.1 Clinical Examination and Palpation
Clinical examination and palpation are essential for diagnosing breast implant flipping. Surgeons use manual techniques to assess implant position, symmetry, and any visible deformities. Palpation helps identify irregularities, such as unnatural firmness or misalignment, which may indicate malposition. Patients may report discomfort or aesthetic concerns, guiding the examination. While palpation is effective for initial assessment, it may not detect all cases of flipping, especially in submuscular implants. Advanced imaging, like ultrasound or MRI, is often recommended for confirmation. Early detection through clinical exams can prevent complications and guide appropriate corrective measures.
5.2 Imaging Techniques (Ultrasound, MRI)
Imaging techniques like ultrasound and MRI are critical for confirming breast implant flipping. Ultrasound provides detailed images of implant position and any malrotation, while MRI offers high-resolution views of soft tissue and implant integrity. These methods help identify subtle shifts or rotations that may not be visible during clinical exams. Advanced imaging is particularly useful for submuscular implants, where palpation alone may be insufficient. Early detection through imaging ensures timely intervention, whether manual correction or surgery is required. These tools are essential for accurate diagnosis and guiding treatment plans to restore proper implant positioning and patient satisfaction.
Manual Correction Techniques
Manual correction involves gentle, external manipulations to reposition flipped implants, restoring proper alignment and aesthetics without surgery, addressing both functional and cosmetic concerns effectively.
6.1 External Manipulation Methods
External manipulation involves gentle, controlled movements to reposition flipped implants. Techniques include targeted pressure and guided exercises to restore proper alignment. Success depends on implant pocket size and tissue flexibility. This non-invasive approach often prevents surgical intervention, offering a quick solution for patients. Skilled practitioners use precise methods to minimize discomfort, ensuring the implant returns to its correct orientation. Regular follow-ups are recommended to maintain stability and prevent recurrence, emphasizing the importance of proper technique and patient compliance in achieving long-term results.
6.2 Implications of Implant Position Changes
Implant position changes can lead to aesthetic concerns, discomfort, and psychological distress. Flipping may cause visible deformities or asymmetry, prompting revision procedures. If left unaddressed, it can result in capsular contracture or seroma. Patients may experience pain, especially if implants shift behind or in front of the muscle. Addressing position changes early is crucial to prevent long-term complications and ensure patient satisfaction. Proper correction techniques are essential to restore both the functional and cosmetic integrity of the implants, maintaining the desired outcomes of the initial surgery.

Preventive Measures
Proper pocket creation and implant selection are crucial to prevent flipping. Surgical expertise and adherence to FDA guidelines ensure optimal placement, minimizing risks of malposition and complications.
7.1 Proper Pocket Creation
Proper pocket creation is critical to prevent breast implant flipping. A well-defined pocket ensures the implant stays in place, reducing the risk of malposition. Surgeons must avoid over-dissection, as this can lead to instability. Studies show that larger pockets increase the likelihood of implant movement. Textured implants, which adhere better to tissue, have lower flip rates compared to smooth ones. Precise surgical techniques and accurate pocket sizing are essential to maintain implant stability and aesthetics. Proper pocket creation minimizes the need for manual correction and reduces the risk of revision surgery, aligning with FDA safety recommendations for breast implant procedures.
7.2 Implant Selection and Placement
Implant selection and placement significantly influence the risk of flipping. Textured implants, which adhere better to surrounding tissue, show lower malposition rates compared to smooth implants. Proper placement, such as behind the muscle, enhances stability and reduces the likelihood of movement. Surgeons must consider patient anatomy and lifestyle when choosing implant type and position. Accurate placement aligns with FDA safety recommendations, minimizing complications. Correct positioning also ensures aesthetic outcomes, reducing the need for manual correction or revision surgery. This approach prioritizes long-term implant stability and patient satisfaction, addressing both functional and cosmetic concerns effectively.
Risks and Complications
Manual flipping can lead to complications like capsular contracture, seroma, and infection. Implant damage or rupture may occur, necessitating surgical intervention to ensure patient safety and aesthetic outcomes.

8.1 Capsular Contracture
Capsular contracture is a common complication following breast implant surgery, often linked to manual flipping. It occurs when the scar tissue around the implant tightens abnormally, causing the breast to harden and become misshapen. This condition can result from inflammation, infection, or improper healing. Manual manipulation of the implant may exacerbate this risk by irritating the surrounding tissue. Symptoms include pain, asymmetry, and a firm texture. Severe cases may require surgical intervention to remove the scar tissue and replace the implant. Preventive measures, such as proper surgical technique and implant selection, are crucial to minimizing this risk.
8.2 Seroma and Infection
Seroma and infection are potential complications following manual flipping of breast implants. A seroma is an accumulation of fluid near the implant, which can occur due to irritation or trauma during manipulation. Infections, such as capsular contracture or implant-related abscesses, may arise if bacteria enter the pocket. Symptoms include swelling, redness, and pain. Antibiotic therapy is often the first line of treatment, but severe cases may require surgical intervention. Proper sterile technique during manual correction is essential to minimize these risks. Patients should monitor for signs of infection and seek immediate medical attention if they occur.
Surgical Intervention
Surgical intervention is required when manual flipping fails, involving pocket adjustment or implant repositioning to restore proper placement and aesthetics, ensuring long-term stability and patient satisfaction.
9.1 When Manual Correction Fails
When manual flipping fails to correct implant malposition, surgical intervention becomes necessary. This typically occurs in cases of severe flipping or rotation, where the implant cannot be repositioned externally. Scar tissue or capsular contracture may also prevent successful manual correction. Surgery involves adjusting the implant pocket, repositioning the implant, or replacing it if damaged. Patients with persistent discomfort or aesthetic concerns often require this step. The procedure ensures proper alignment and restores both the functional and aesthetic outcomes of the implant. Experienced surgeons are crucial for achieving optimal results and minimizing further complications.
9.2 Surgical Techniques for Correction
Surgical correction for failed manual flipping involves adjusting the implant pocket or repositioning the implant. Techniques may include capsulotomy (scar tissue release) or capsulectomy (removal of scar tissue) to ensure proper alignment. In some cases, implant replacement is necessary if damage occurs. Surgeons may also tighten the pocket to prevent future malposition. These procedures are tailored to address the specific cause of flipping, ensuring both aesthetic and functional restoration. Experienced surgeons use precise methods to minimize complications and achieve long-term stability for the patient.
Psychological Impact on Patients
Breast implant flipping can cause significant anxiety and dissatisfaction, affecting a patient’s self-perception and confidence. Emotional distress often arises from unexpected changes in appearance and the need for correction.
10.1 Patient Anxiety and Satisfaction
Breast implant flipping often leads to significant patient anxiety, as the unexpected change in appearance can undermine confidence and self-perception. Many patients express dissatisfaction, feeling distressed by the loss of their desired aesthetic outcome. Emotional distress may intensify if the issue recurs or requires multiple corrections. The psychological impact can be profound, affecting overall well-being and body image. Addressing these concerns through counseling and clear communication is crucial to restoring patient satisfaction and trust in their surgical outcomes.
10.2 Counseling and Support
Counseling plays a vital role in addressing the emotional and psychological impact of breast implant flipping. Patients often experience heightened anxiety and uncertainty, requiring empathetic support to alleviate fears. Surgeons and healthcare providers should provide clear communication, reassurance, and education about the condition and its solutions. Offering resources for emotional support and connecting patients with others who have undergone similar experiences can foster a sense of community and understanding. This holistic approach helps patients regain confidence and make informed decisions about their care, ensuring both emotional and physical well-being are prioritized.
Case Studies and Statistics
Studies reveal a 5.9% flip rate in smooth round implants versus 1.4% in textured anatomical ones, highlighting significant disparities in implant stability and patient outcomes.
11.1 Real-World Examples
A patient with smooth round implants experienced flipping post-revision surgery, corrected manually. Another case involved a viral video showing a botched implant flipping. Studies reveal a 5.9% flip rate in smooth implants versus 1.4% in textured ones, emphasizing higher risks with smooth designs. These examples highlight the prevalence and challenges of implant malposition, underscoring the need for careful surgical techniques and patient monitoring to minimize complications and improve outcomes in breast augmentation procedures.
11.2 Incidence Rates and Trends
Studies reveal varying incidence rates of breast implant flipping, with smooth round implants showing a higher rate of 5.9% compared to 1.4% for textured anatomical devices. A retrospective analysis of 165 patients reported a 5.5% flip rate, highlighting implant type as a significant factor. Trends indicate that smooth implants are more prone to malposition due to their design, while textured implants exhibit greater stability. These findings underscore the importance of implant selection and surgical technique in minimizing complications, with data suggesting a consistent pattern over time in implant behavior and patient outcomes.

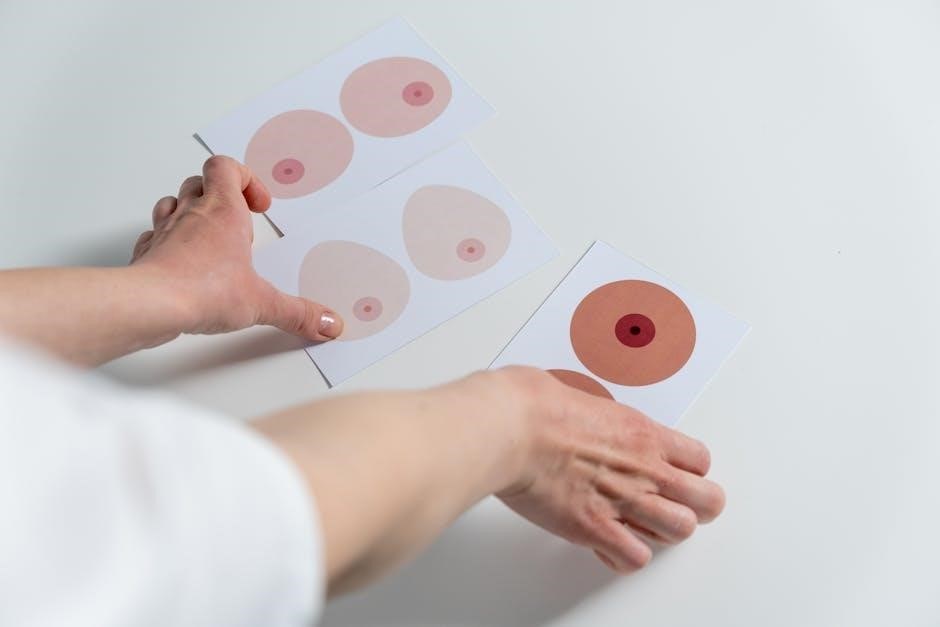
Comparing Smooth and Textured Implants
Smooth round implants show higher flipping rates (5.9%) compared to textured anatomical implants (1.4%). Design differences influence stability, with textured implants offering better resistance to malposition.
12.1 Smooth Round Implants
Smooth round implants are more prone to flipping due to their design, which allows for natural movement within the breast pocket. Studies show a higher incidence of malposition in smooth round implants (5.9%) compared to textured anatomical ones (1.4%). This is attributed to their lack of surface texture, which reduces resistance to movement. Manual correction is often feasible, but improper pocket size and surgical technique can exacerbate the issue. Patients with larger implants or submuscular placements are at higher risk. Regular monitoring and proper placement are crucial to minimize flipping and ensure long-term stability.
12.2 Textured Anatomical Implants
Textured anatomical implants exhibit lower malposition rates compared to smooth round implants, with studies showing a 1.4% incidence of flipping. Their design, featuring a textured surface and teardrop shape, promotes better tissue adherence, reducing the likelihood of rotation or flipping. The textured surface creates friction, stabilizing the implant within the breast pocket. This design minimizes the need for manual correction and enhances long-term stability. However, proper surgical technique remains critical to ensure optimal placement and minimize complications, as improper positioning can still lead to malposition despite the implant’s design advantages.
The Role of Plastic Surgeons
Plastic surgeons play a crucial role in manually flipping breast implants, utilizing their expertise to correct malposition and ensure proper placement, while also educating patients on post-surgical care.
13.1 Surgical Expertise
Surgical expertise is critical in addressing breast implant flipping, as plastic surgeons must possess the skill to manually correct malposition while minimizing complications. Their ability to assess implant type, pocket size, and tissue integrity ensures precise manipulation. Surgeons with extensive experience in breast reconstruction and revision surgeries are better equipped to handle complex cases, such as implants that have flipped or rotated. Proper training and familiarity with both smooth and textured implants allow them to apply the right technique, whether it’s external manipulation or surgical intervention, to restore aesthetic and functional outcomes for patients.
13.2 Patient Education
Patient education plays a vital role in managing breast implant flipping. Surgeons must inform patients about the risks, signs, and prevention strategies. Educating patients on proper post-operative care, such as avoiding strenuous activities, can reduce the likelihood of implant malposition. Additionally, patients should be aware of the importance of regular follow-ups to monitor implant position. Clear communication about the differences between smooth and textured implants, as well as their respective flip rates, empowers patients to make informed decisions. This proactive approach fosters trust and ensures patients are proactive in maintaining their surgical outcomes, aligning with FDA recommendations for implant safety.
FDA Updates and Regulations
The FDA has strengthened safety requirements for breast implants, updating study results and monitoring procedures to address malposition risks, ensuring patient safety and informed decision-making.
14.1 Safety Requirements
The FDA has implemented stricter safety measures for breast implants, including updated study results and enhanced monitoring protocols. These regulations aim to reduce malposition risks and ensure patient safety. Manufacturers are now required to provide detailed labeling and tracking information. The FDA emphasizes the importance of patient-specific data to improve outcomes. These updates reflect a commitment to addressing implant-related complications, ensuring transparency, and fostering informed decision-making for those considering breast augmentation or revision surgeries.
14.2 Study Results and Recommendations
Recent studies highlight that smooth round implants have a higher malposition rate (5.9%) compared to textured anatomical ones (1.4%). The FDA recommends enhanced patient monitoring and detailed documentation to reduce risks. Manufacturers are advised to improve implant design for stability. Patients are encouraged to follow post-operative care diligently. These findings underscore the importance of proper surgical techniques and implant selection to minimize complications. The FDA also advocates for ongoing research to refine safety protocols and ensure better outcomes for individuals undergoing breast implant procedures.
Future Technological Advancements
Innovative implant designs, such as double-lumen implants, aim to reduce flipping risks. Smart implants with monitoring systems may soon detect malposition early, enhancing patient safety and outcomes.
15.1 Innovative Implant Designs
Innovative implant designs, such as double-lumen implants, aim to minimize flipping risks by providing structural stability. These implants feature a silicone prosthesis within a saline-filled outer layer, reducing the likelihood of malposition. Additionally, advancements in textured surfaces and anatomical shapes help maintain proper orientation. Researchers are also exploring smart implants with embedded sensors to monitor position and detect early signs of flipping. Such designs not only enhance safety but also improve aesthetic outcomes, addressing both patient and surgeon concerns effectively.
15.2 Smart Implants and Monitoring
Smart implants with embedded sensors are revolutionizing breast implant monitoring. These devices can detect early signs of flipping or malposition, providing real-time data to surgeons. Advanced monitoring systems enable remote tracking of implant orientation, reducing the need for frequent clinical visits. Such technologies not only improve patient safety but also offer peace of mind. By integrating innovative materials and IoT capabilities, smart implants are paving the way for proactive care, ensuring optimal outcomes and minimizing complications related to manual flipping or rotation.
Manual flipping of breast implants is a manageable issue with proper techniques and patient-surgeon collaboration, emphasizing prevention and early detection for optimal outcomes and patient satisfaction.
16.1 Summary of Key Points
Manual flipping of breast implants involves correcting unintended rotation or malposition, often addressed through gentle manipulation or surgical intervention. Studies show higher flip rates in smooth round implants compared to textured anatomical ones. Proper pocket creation, implant selection, and surgical technique are critical in preventing malposition. Patient-related factors, such as anatomy and activity level, also play a role. Early detection and correction are essential to avoid complications like capsular contracture or seroma. Surgeons emphasize the importance of education and regular follow-ups to ensure optimal outcomes and patient satisfaction.






